Abstract
Research Article
Association of Toll-like receptor 2, 4, and 9 gene polymorphism with high altitude induced thrombosis patients in Indian population
Swati Sharma, Iti Garg*, Gauri Mishra, Babita Kumari, Lilly Ganju and Bhuvnesh Kumar
Published: 08 February, 2019 | Volume 3 - Issue 1 | Pages: 006-015
Venous Thromboembolism (VTE) is a multifactorial disease that is influenced by individual genetic background and various environmental factors, high altitude (HA) being the one. HA exposure may cause release of several damage associated molecular patterns (DAMPs), which act as ligand for various immune receptors. Previous studies on western population involving SNPs analysis of TLRs demonstrated that TLRs are involved in development and progression of several cardiovascular diseases. But, no such study has been done in Indian population in context of HA exposure. TLRs, being receptors play a significant role in manifestation and elimination of diseases by recognition of specific ligands and downstream signal transduction therefore; the genetic variation in TLRs could be implicated for imparting varying response of individuals to discrete diseases.
Therefore, in accordance with it, in present study changes in protein structures of TLR2 and TLR4 due to presence of SNP were accessed by in-silico tools to observe whether the mutation has effect on protein structure and integrity which further influencing its function. The results showed that SNP harbouring protein has decreased functional pockets, thus may be protective for disease. Taking this lead further to genotypic level, first time association between Toll-like receptor genes polymorphism and risk of high altitude induced venous thrombosis is analyzed in Indian population by PCR RFLP method. Though the result showed initial trend that TLR2 and TLR9 SNP are monomrphic in distribution and for TLR4 there was no significant difference in distribution of SNP between healthy and HA-DVT group, these SNPs have potential to be used as susceptibility markers if studied in large population size.
Read Full Article HTML DOI: 10.29328/journal.icci.1001008 Cite this Article Read Full Article PDF
Keywords:
VTE; TLRs; SNP; Genotyping
References
- Homans J. Thrombosis of the deep leg veins due to prolonged sitting. N Engl J Med. 1954; 250: 148-149. Ref.: https://goo.gl/za8FH9
- Gibbs NM. Venous thrombosis of the lower limbs with particular to bed rest. Br J Surg. 1957; 45: 209-236. Ref.: https://goo.gl/t2j1EN
- Hull RD, Raskob GE. Prophylaxis of venous thromboembolic disease following hip and knee surgery. J Bone Joint Surg Am.1986; 68: 146-150. Ref.: https://goo.gl/RN48ra
- Ward M. Mountain Medicine: A Clinical Study of Cold and High Altitude. 1975; Ref.: https://goo.gl/dDt4Ab
- Zangari M, Fink L, Tolomelli G, Lee JC, Stein BL, et al. Could hypoxia increase the prevalence of thrombotic complications in polycythemia vera? Blood Coagul Fibrinolysis. 2013; 24: 311-316. Ref.: https://goo.gl/8UkEK6
- Anand AC, Saha A, Kumar R, Sharma V, Jha SK. Portal system thrombosis: a new dimension of high altitude illnesses. Trop Gastroenterol. 2000; 21: 172-173. Ref.: https://goo.gl/FrQesU
- Cheng S, Chng SM, Singh R. Cerebral venous infarction during a high altitude expedition. Singapore Med J. 2009; 50: e306-308. Ref.: https://goo.gl/Txhhdz
- Gupta N, Ashraf MZ. Exposure to high altitude: a risk factor for venous thromboembolism? Semin Thromb Hemost. 2012; 38: 156-163. Ref.: https://goo.gl/MdT1w6
- Anand AC, Jha SK, Saha A, Sharma V, Adya CM. Thrombosis as a complication of extended stay at high altitude. Natl Med J India. 2001; 14: 197-201 Ref.: https://goo.gl/3pLNJg
- White RH, Zhou H, Romano PS. Incidence of idiopathic deep vein thrombosis and secondary thromboembolism among ethnic groups in California. Ann Inter Med. 1998; 128: 737-740. Ref.: https://goo.gl/vuUKa1
- Kapoor VK. Venous thromboembolism in India. Editorials. Natl Med J India. 2010; 23: 93-95.
- Griffin JH, Evatt B, Zimmerman TS. Deficiency of protein C in congenital thrombotic disease. J Clin Invest. 1981; 68: 1370-1373. Ref.: https://goo.gl/FxEHjB
- Koster T, Rosendaal FR, Briët E, van der Meer FJ, Colly LP, et al. Protein C deficiency in a controlled series of unselected outpatients: an infrequent but clear risk factor for venous thrombosis (Leiden Thrombophilia Study). Blood. 1995; 85: 2756-2761. Ref.: https://goo.gl/fFLbzx
- Bezemer ID, Rosendaal FR. Predictive genetic variants for venous thrombosis: what’s new? Semin Hematol. 2007; 44: 85-92. Ref.: https://goo.gl/khg4Q2
- Heit JA, Armasu SM, Asmann YW, Cunningham JM, Matsumoto ME, et al. A genome-wide association study of venous thromboembolism identifies risk variants in chromosomes 1q24.2 and 9q. J Thromb Haemost. 2012; 10: 1521-1531. Ref.: https://goo.gl/Qswtwx
- Mannucci PM, Gringeri A, Peyvandi F, Di Paolantonio T, Mariani G. Short-term exposure to high altitude causes coagulation activation and inhibits fibrinolysis. Thromb Haemost. 2002; 87: 342-343. Ref.: https://goo.gl/Asrhok
- Eltzschig HK, Carmeliet P. Hypoxia and inflammation. N Engl J Med. 2011; 364: 656-665. Ref.: https://goo.gl/ea8Ncw
- Frantz S, Ertl G, Bauersachs J. Mechanism of disease: Toll Like Receptors in cardiovascular diseases. Nat Clin Pract Cardiovasc Med. 2007; 4: 444–454. Ref.: https://goo.gl/JfJP2m
- Hamann L, Gomma A, Schröder NW, Stamme C, Glaeser C, et al. A frequent Toll like receptor (TLR) 2 polymorphism is a risk factor for coronary restenosis. J Mol Med. 2005; 83: 478–485. Ref.: https://goo.gl/LLYXTW
- Kiechl S, Lorenz E, Reindl M, Wiedermann CJ, Oberhollenzer F, et al. Toll-like receptor 4 polymorphism and atherogenesis. N Engl J Med. 2002; 347:185–192. Ref.: https://goo.gl/o3xEaa
- Hodgkinson CP1, Ye S. Toll-like receptors, their ligands, and atherosclerosis. Sci World J. 2011; 11: 437–453. Ref.: https://goo.gl/K62h2M
- Hamann L, Glaeser C, Hamprecht A, Gross M, Gomma A, et al. Toll-like receptor (TLR)-9 promotor polymorphisms and atherosclerosis. Clin Chim Acta. 2006; 364: 303–307. Ref.: https://goo.gl/LorUDw
- Källberg M, Wang H, Wang S, Peng J, Wang Z, et al. Template-based protein structure modeling using the RaptorX web server. Nature Protocols. 2012; 7: 1511–1522. Ref.: https://goo.gl/GLBAzG
- Källberg M, Wang H, Wang S, Peng J, Wang Z, et al. Template-based protein structure modeling using the RaptorX web server. Nature Protocols. 2012; 7: 1511–1522. Ref.: https://goo.gl/fuefUb
- Wiederstein M, Sippl MJ. ProSA-web: interactive web service for the recognition of errors in three-dimensional structures of proteins. Nucleic Acids Research. 2007; 35: W407-W410. Ref.: https://goo.gl/57YcWa
- Sippl MJ. Recognition of Errors in Three-Dimensional Structures of Proteins. Proteins. 1993; 17: 355-362. Ref.: https://goo.gl/EuZEie
- Laskowski RA, Moss DS, Thornton JM. Main-chain bond lengths and bondangles in protein structures. J Mol Biol. 1993; 231: 1049–1067. Ref.: https://goo.gl/csfJh2
- Dundas J, Ouyang Z, Tseng J, Binkowski A, Turpaz Y, et al. CASTp:computed atlas of surface topography of proteins with structural and topographical mapping of functionally annotated residues. Nucleic Acids Res 2006, 34(Web Server issue): W116–W118. Ref.: https://goo.gl/F8n6Qn
- Laskowski RA, Watson JD, Thornton JM. ProFunc: a server for predicting protein function from 3D structure. Nucleic Acids Res. 2005; 33 (Web Server issue): W89–W93. Ref.: https://goo.gl/q6AzY5
- Capriotti E, Calabrese R, Casadio R. Predicting the insurgence of human genetic diseases associated to single point protein mutations with support vector machines and evolutionary information. Bioinformatics. 2006; 22: 2729–2734. Ref.: https://goo.gl/SU8AC5
- Kim JK, Cho Y, Lee M, Laskowski RA, Ryu SE, et al. BetaCavityWeb: a webserver for molecular voids and channels. Nucleic Acids Res. 2015; W413-418. Ref.: https://goo.gl/hthiKx
- Libby P, Simon DI. Inflammation and Thrombosis. The Clot Thickens. Circulation. 2001; 103: 1718-1720. Ref.: https://goo.gl/pWiZgg
- Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002; 105: 1135–1143. Ref.: https://goo.gl/j5Ym2X
- Zebrack JS, Anderson JL. The role of inflammation and infection in the pathogenesis and evolution of coronary artery disease. Current Cardiology Reports. 2002; 4: 278–288. Ref.: https://goo.gl/pcjdUZ
- Liu F, Lu W, Qian Q, Qi W, Hu J, et al. Frequency of TLR 2, 4, and 9 Gene Polymorphisms in Chinese Population and Their Susceptibility to Type 2 Diabetes and Coronary Artery Disease. J Biomed Biotechnol. 2012; 2012: Article ID 373945. Ref.: https://goo.gl/CHHgq3
- Medzhitov R, Preston-Hurlburt P, Janeway CA Jr. A human homologue of the Drosophila toll protein signals activation of adaptive immunity. Nature. 1997; 388: 394–397. Ref.: https://goo.gl/8FS3AK
- Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006; 124: 783–801. Ref.: https://goo.gl/eyckzd
- Uematsu S, Akira S. Toll-like receptors and innate immunity. J Mol Med (Berl). 2006; 84: 712–725. Ref.: https://goo.gl/2gN9rC
- Kiechl S, Lorenz E, Reindl M, Wiedermann CJ, Oberhollenzer F, et al. Toll-like receptor 4 polymorphisms and atherogenesis. The New England Journal of Medicinel. 2002; 347: 185–192. Ref.: https://goo.gl/hujrpw
- Hollestelle SC, De Vries MR, Van Keulen JK, Schoneveld AH, Vink A, et al. Toll-like receptor 4 is involved in outward arterial remodeling. Circulation. 2004; 109: 393–398. Ref.: https://goo.gl/NcqXx1
- Boekholdt SM, Agema WR, Peters RJ, Zwinderman AH, van der Wall EE, et al. Variants of toll-like receptor 4 modify the efficacy of statin therapy and the risk of cardiovascular events. Circulation. 2003; 107: 2416–2421. Ref.: https://goo.gl/RLGTh4
- Kolek MJ, Carlquist JF, Muhlestein JB, Whiting BM, Horne BD, et al. Toll-like receptor 4 gene Asp299Gly polymorphism is associated with reductions in vascular inflammation, angiographic coronary artery disease, and clinical diabetes. Am Heart J. 2004; 148: 1034–1040. Ref.: https://goo.gl/vqUa9r
- Hang J, Zhou W, Zhang H, Sun B, Dai H, et al. TLR4 Asp299Gly and Thr399Ile polymorphims are very rare in the Chinese population. J Endotoxin Res. 2004; 10: 238–240. Ref.: https://goo.gl/jiwGNY
- Lin YC, Chang YM, Yu JM, Yen JH, Chang JG, et al. Toll-like receptor 4 gene C119A but not Asp299Gly polymorphism is associated with ischemic stroke among ethnic Chinese in Taiwan. Atherosclerosis. 2005; 180: 305–309. Ref.: https://goo.gl/TTi92x
- Hur JW, Shin HD, Park BL, Kim LH, Kim SY, et al. Association study of Toll-like receptor 9 gene polymorphism in Korean patients with systemic lupus erythematosus. Tissue Antigens. 2005; 65: 266–270. Ref.: https://goo.gl/nD33Eq
- Tao K, Fujii M, Tsukumo SI, Maekawa Y, Kishihara K, et al. Genetic variations of Toll-like receptor 9 predispose to systemic lupus erythematosus in Japanese population. Annals of the Rheumatic Diseases. 2007; 66: 905–909. Ref.: https://goo.gl/gkwdsb
- Ng MW, Lau CS, Chan TM, Wong WH, Lau YL. Polymorphisms of the toll-like receptor 9 (TLR9) gene with systemic lupus erythematosus in Chinese. Rheumatology. 2005; 44: 1456–1457. Ref.: https://goo.gl/NoayCf
Figures:

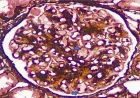
Figure 1

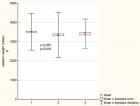
Figure 2

Figure 3

Figure 4

Figure 5

Figure 6
Similar Articles
-
Association of Toll-like receptor 2, 4, and 9 gene polymorphism with high altitude induced thrombosis patients in Indian populationSwati Sharma,Iti Garg*,Gauri Mishra,Babita Kumari,Lilly Ganju,Bhuvnesh Kumar. Association of Toll-like receptor 2, 4, and 9 gene polymorphism with high altitude induced thrombosis patients in Indian population. . 2019 doi: 10.29328/journal.icci.1001008; 3: 006-015
Recently Viewed
-
Transumbilical Single-incision Hiatal Hernia Repair and Nissen Fundoplication in situs Inversus Totalis: A Rare Case ReportQing Cao,Chen Kang,Kang Gu,Yin Peng,Yang Lv,Xu-Zhong Ding,Peng Li*. Transumbilical Single-incision Hiatal Hernia Repair and Nissen Fundoplication in situs Inversus Totalis: A Rare Case Report. Adv Treat ENT Disord. 2026: doi: 10.29328/journal.ated.1001017; 10: 001-003
-
NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and MuscleRizwan Uppal,Umar Saeed*,Muhammad Rehan Uppal. NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and Muscle. Ann Clin Endocrinol Metabol. 2026: doi: 10.29328/journal.acem.1001032; 10: 001-009
-
Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical TrialAnders Wänman*, Susanna Marklund, Negin Yekkalam. Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical Trial. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001046; 9: 001-008
-
Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and GermanyJochen Hardt*,Lisa Weyer,Malgorzata Dragan,Wilfried Laubach. Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and Germany. Insights Depress Anxiety. 2017: doi: 10.29328/journal.hda.1001003; 1: 015-022
-
Case Report of a Child with Beta Thalassemia Major in a Tribal Region of IndiaNeha Chauhan, Prakash Narayan, Mahesh Narayan, Manisha Shukla*. Case Report of a Child with Beta Thalassemia Major in a Tribal Region of India. J Child Adult Vaccines Immunol. 2023: doi: 10.29328/journal.jcavi.1001011; 7: 005-007
Most Viewed
-
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)Dasse Sery Romuald*, KL Siransy, N Koffi, RO Yeboah, EK Nguessan, HA Adou, VP Goran-Kouacou, AU Assi, JY Seri, S Moussa, D Oura, CL Memel, H Koya, E Atoukoula. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024 doi: 10.29328/journal.aaai.1001035; 8: 007-012
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037
-
Snow white: an allergic girl?Oreste Vittore Brenna*. Snow white: an allergic girl?. Arch Asthma Allergy Immunol. 2022 doi: 10.29328/journal.aaai.1001029; 6: 001-002
-
Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disordersElena Viktorovna Drozdova*. Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disorders. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001028; 5: 038-040

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."